This World Diabetes Day (Nov 14), India ranks high in the list of developing countries with the greatest number of people affected with diabetes. Estimates from the World Diabetes Atlas and the WHO records place India in the top ten countries in the world with the highest burden of Type 2 diabetes mellitus (T2D).
- Projected numbers for diabetes in the Indian population – 87 million by the year 2030;
- Highest prevalence found in the urban regions, when compared to semi-urban and rural areas;
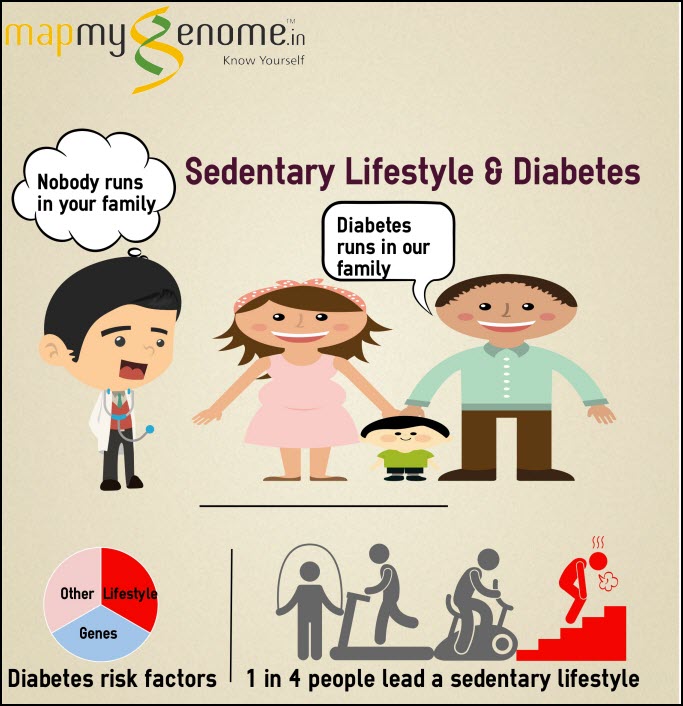
- ”Asian Indian” phenotype associated with greater risk and earlier onset for T2D (a decade earlier than Europeans) – clinical features include increased visceral fat and serum triglycerides, low HDL-levels Type 2 diabetes is a ”multifactorial” disorder, which means that a complex interplay between genetic and environmental factors underlies the etiology of this condition. Individuals clinically diagnosed with T2D complain of a lifelong burden in terms of daily medications, associated liver and kidney complications and dietary restrictions. There is no proven cure for T2D, only ”management” through Since a majority of T2D’s symptoms can be managed through epigenetic intervention, physicians have started calling it a ”lifestyle syndrome”.
Why genetic screening is a useful tool – The science behind the ”sugar disease”
T2D is caused by impaired insulin secretion by the β islet cells of the pancreas. Insulin is a very important hormone for metabolic function, and is a key component of glucose ”homeostasis” (state of balance). While investigating the mechanisms behind T2D development and physiology, scientists have discovered at least 20 important loci (gene locations) which are linked with insulin function/insulin sensitivity.
Single base variations in the sequence of these genes, called Single Nucleotide Polymorphisms (SNPs, pronounced ”snips”) increase an individual’s risk for developing T2D. Screening for all known variations is an uphill task and reduces accuracy. However, large-scale population studies in Indians and Caucasians have successfully elucidated reliable results to help narrow down causal variants which will provide accurate risk scores.
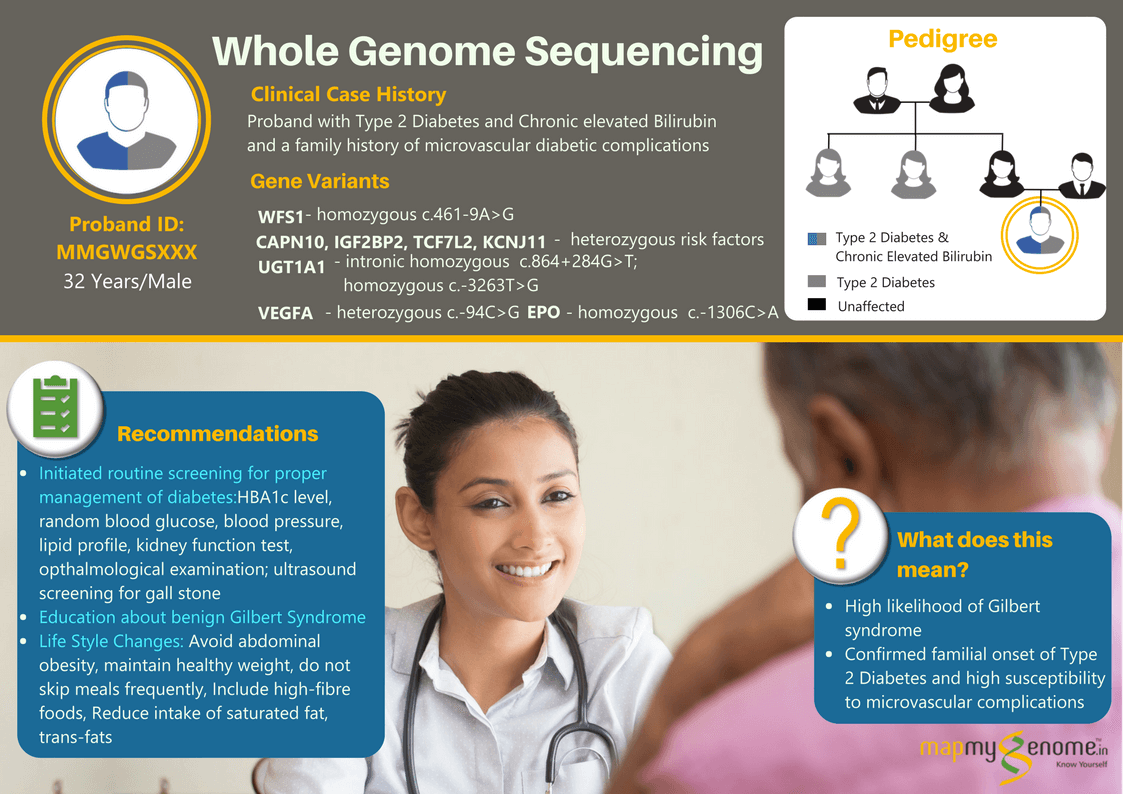
KCNQ1 and KCNJ11 : These genes produce proteins which are present in the potassium ion channels of the pancreatic β cells, thereby playing a vital role in insulin secretion.
PPARγ and FTO: PPARγ is found in the adipose tissue and improper gene function causes insulin resistance. This leads to metabolic diseases, diabetes among others. FTO gene product is a regulator of fat storage, transport and metabolism.
TCF7L2, HHEX-IDE, CDKAL1 and IGF2BP2 : Variations in these genes have been found in diabetic patients in Indian population. When insulin resistance develops, secretion by the β cells does not happen according to the level of insulin in the body, resulting in a deficiency of the hormone.
Scientific findings from T2D-based studies have shown to be consistent across different races and ethnicities, for the genes mentioned above. A screening procedure that analyzes variations in these loci is useful to identify high-risk individuals, to facilitate early intervention and/or delay onset.
Some Do’s and Don’ts
References:
-
Sicree R, Shaw J, Zimmet P. Diabetes and impaired glucose tolerance. In: Gan D, editor.Diabetes atlas.4th ed. International Diabetes Federation. Belgium: International Diabetes Federation; 2009. pp. 1–105.
-
Mohan V, Radhika G, Vijayalakshmi P, Sudha V. Can the diabetes/cardiovascular disease epidemic in India be explained, at least in part, by excess refined grain (rice) intake? 2010.