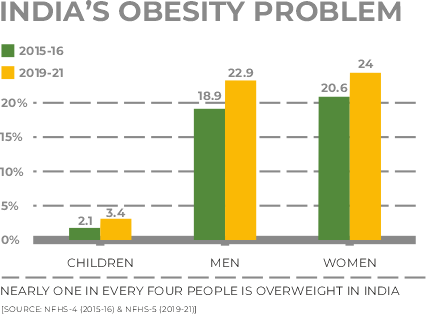
Obesity is one of the most prevailing health conditions in people of all ages. A significant rise in obesity cases is due to unhealthy lifestyles. According to World Health Organisation (WHO), obesity has nearly tripled worldwide since 1975. Yes! Can blame it on all the finger-lickin’ junk foods for those extra kilos.
But numerous researchers have already found that our genes can be a predisposing factor for obesity.
What is Obesity?
Obesity is commonly defined as having a higher body mass index. According to the Center for Disease Control and Prevention (CDC), a BMI of more than 30 is considered obese. Obesity is not a cosmetic issue. However, obesity can be a primary cause of many diseases like cardiovascular diseases, diabetes, a few cancers, and many more.
The table shows the weight status of people based on different BMI values. The weight statuses are the same for men and women of all body types and ages.
| BMI Value | Weight Status |
| Below 18.5 | Underweight |
| 18.5 – 24.9 | Healthy Weight |
| 25.0 – 29.9 | Overweight |
| 30.0 and Above | Obesity |
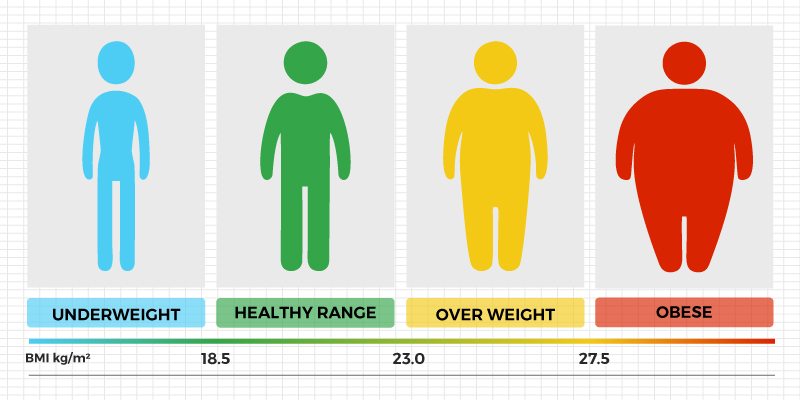
BMI is calculated by a person’s weight in kilograms (or pounds) divided by the square of height in meters (or feet). Many BMI calculators are available online for free.
What Causes Obesity?
Below are some major factors contributing to obesity:
- Diet and eating patterns: A diet with high-calorie food and beverages, fewer vegetables and fruits, and a lot of junk foods can cause a calorie imbalance and lead to weight gain. Frequent snacking and lack of proper meal timings are also associated with weight gain.
- Physical activity: People with a sedentary lifestyle tend to spend fewer calories, which eventually are stored as fat, leading to weight gain.
- Sleep routines: Research has found that short sleep duration results in metabolic changes that may be linked to obesity.
- Medication and Illnesses: Few medications, such as steroids and some antidepressants, may cause weight gain. Illnesses like Cushing’s disease may lead to weight gain or obesity.
How is Genetics Related to Obesity?
Obesity is closely linked to genetic factors. The gene frequently associated with predisposition to obesity is FTO ( fat-mass and obesity-related).
Single Nucleotide Polymorphisms or SNPs are the common genetic variation in human DNA. Some variants are associated with an increased risk for obesity/weight gain. How these genes/SNPs can influence weight gain is still unclear. But a lot of studies show that it plays a role in influencing brain circuits that regulate our appetite, energy balance, and intake of food. The FTO gene is highly expressed in the brain.
Multiple SNP’s on multiple genes can increase an individual's obesity/weight gain risk. But let’s not go there for now.
RS Numbers
We denote individual SNPs with special codes called ‘rs numbers.’
The rs993609 SNP is the most studied SNP within the FTO gene and is associated with the greatest risk of weight gain. This SNP causes a change in the FTO gene sequence from the letter “T” to the letter “A.” The variation in the sequence from “T” to “A” results in an increased risk for obesity. As we inherit two copies of each gene (one from the father and one from the mother), three genetic combinations ( genotypes ) are possible at this particular location, AA, AT, and TT.
One study found that people with the “AA” genotype weigh on average 3 kg more than those with the TT genotype. People with the “AT” genotype are around 1.5 kg more than those with the TT genotype.
Some studies show that the ‘A’ allele (alternative forms of a gene that arise by mutation/variation and are found at the same place on the chromosome ) alters the activity of brain circuits that control appetite and responsiveness to food. Individuals carrying the obesity-susceptible ‘A’ allele of the FTO gene tend to have a larger appetite. They are less likely to feel full after a meal.
The ‘Hunger’ Hormone
Research suggests that individuals with the “A” allele were highly responsive to Ghrelin - an appetite-stimulating hormone released by the pancreas, stomach, and small intestine. Ghrelin sends signals to the brain to make us feel hungry.
Usually, ghrelin secretion is stopped after a meal, making us feel full. But individuals with the “A” allele tend to have raised ghrelin levels and lower leptin (appetite-suppressing hormone)levels. Higher ghrelin levels and lower leptin levels might contribute to higher food cravings.
Can Genetics Help in Obesity Prevention?
People can be genetically predisposed to weight gain/obesity. But following a healthy diet and increasing physical activity can decrease an individual's risk for obesity.
So, it is essential for everyone, especially those with a family history of obesity, cardiovascular diseases, or diabetes, to know their genetic predisposition to these conditions and take appropriate action to prevent obesity.
With more than 20 years of experience in genomics and a highly skilled bioinformatics team, Mapmygenome has curated highly validated SNPs and made preventive genomics products like MyFitGene.
MyFitGene is Mapmygenome’s DNA-based sports & fitness solution. This preventive genomics solution provides 40+ easy-to-read reports on fitness, nutrition, and wellness. You will be able to personalize your training regimen and diet plan. This solution includes free genetic counselling and personalised recommendations to upgrade to an effective fitness routine.
For more details: Click on MyFitGene or Call Us at 1800-102-4595 or WhatsApp at 86883 10052.
Reference :
Taheri, S. “The Link between Short Sleep Duration and Obesity: We Should Recommend More Sleep to Prevent Obesity - PMC.” PubMed Central (PMC), www.ncbi.nlm.nih.gov, 17 July 2006, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2082964/.
Frayling, Timothy M., et al. “A Common Variant in the FTO Gene Is Associated with Body Mass Index and Predisposes to Childhood and Adult Obesity - PMC.” PubMed Central (PMC), www.ncbi.nlm.nih.gov, 12 Apr. 2007, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2646098/.
Karra, Efthimia, et al. “A Link between FTO, Ghrelin, and Impaired Brain Food-Cue Responsivity - PMC.” PubMed Central (PMC), www.ncbi.nlm.nih.gov, 15 July 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3726147/.