Mitochondria, the powerhouses of our cells, play an indispensable role in energy production. However, when these energy factories malfunction due to genetic mutations, a wide array of health issues known as mitochondrial diseases can arise. In this in-depth guide, we'll delve deeper into the complexities of these disorders, shedding light on their causes, symptoms, and potential treatments, while providing a comprehensive overview of the various diseases that fall under this umbrella.
What are Mitochondrial Diseases?
Mitochondrial diseases are a heterogeneous group of disorders caused by defects in the genetic material (DNA) housed within mitochondria. These mutations can impair the mitochondria's ability to produce energy efficiently, leading to a broad spectrum of symptoms that can affect virtually any organ or tissue in the body.
Causes of Mitochondrial Diseases
Mitochondrial diseases can be either inherited or acquired:
- Inherited: These mutations are passed down from parents to children, often through the mother's mitochondrial DNA (mtDNA).
- Acquired: These mutations develop sporadically during a person's lifetime due to environmental factors or other unknown causes.
Symptoms of Mitochondrial Diseases
The symptoms of mitochondrial diseases are incredibly diverse, ranging from mild to severe and affecting different organs and systems:
- Muscle weakness and fatigue: As muscles require a significant amount of energy, muscle weakness and fatigue are common symptoms.
- Exercise intolerance: Individuals with mitochondrial diseases may experience fatigue and exhaustion during physical activity.
- Neurological problems: These can include seizures, developmental delays, dementia, vision and hearing loss, migraines, strokes, movement disorders, and cognitive impairment.
- Cardiomyopathy: Mitochondrial dysfunction can weaken the heart muscle, leading to cardiomyopathy and rhythm abnormalities.
- Gastrointestinal issues: Symptoms like swallowing difficulties, constipation, diarrhea, gastrointestinal pain, and gastroparesis (delayed stomach emptying) can occur.
- Liver and kidney dysfunction: Mitochondrial diseases can affect the function of these vital organs, leading to liver failure and kidney disease.
- Diabetes and other metabolic disorders: Impaired energy production can disrupt metabolic processes, contributing to conditions like diabetes, hypoglycemia, and lactic acidosis (buildup of lactic acid in the blood).
Comprehensive List of Mitochondrial Diseases
The following list encompasses a wide range of mitochondrial diseases, categorized based on their primary affected systems and includes additional details on each:
Neurological
- MELAS (Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like episodes): Characterized by stroke-like episodes, seizures, muscle weakness, and lactic acidosis.
- Kearns-Sayre Syndrome (KSS): A multisystem disorder with progressive external ophthalmoplegia (weakness of eye muscles), pigmentary retinopathy (eye disease), and heart conduction defects.
- Leigh Syndrome: A severe neurological disorder affecting the central nervous system, often with early onset in infancy or childhood, causing developmental delays, seizures, and movement disorders.
- MERRF (Myoclonic Epilepsy with Ragged-Red Fibers): A progressive disorder characterized by myoclonus (muscle jerks), epilepsy, ataxia (uncoordinated movements), and muscle weakness.
- LHON (Leber's Hereditary Optic Neuropathy): A form of vision loss that primarily affects young adults, causing painless loss of central vision.
- NARP (Neuropathy, Ataxia, and Retinitis Pigmentosa): A neurodegenerative disorder with ataxia, sensory neuropathy (numbness and tingling in the extremities), and retinitis pigmentosa.
- MNGIE (Mitochondrial Neurogastrointestinal Encephalomyopathy): A rare disorder characterized by gastrointestinal dysmotility, cachexia (wasting), and neurological symptoms like ptosis and peripheral neuropathy.
- Alpers-Huttenlocher Syndrome: A rare, progressive neurodegenerative disorder usually presenting in infancy or early childhood with liver disease, seizures, and developmental regression.
Muscular
- Mitochondrial Myopathies: A group of disorders primarily affecting the muscles, causing muscle weakness, fatigue, and exercise intolerance.
- CPEO (Chronic Progressive External Ophthalmoplegia): A disorder characterized by slowly progressive paralysis of the eye muscles, often associated with ptosis (drooping eyelids) and double vision.
Multi-systemic
- Pearson Syndrome: A rare, multisystem disorder that typically presents in infancy with bone marrow dysfunction, exocrine pancreatic insufficiency, and lactic acidosis.
- Mitochondrial DNA Depletion Syndrome (MDS): A group of disorders caused by a significant decrease in the amount of mitochondrial DNA in various tissues, affecting multiple organs and systems with a wide range of symptoms.
- 3-Methylglutaconic Aciduria (3-MGA): A group of disorders characterized by elevated levels of 3-methylglutaconic acid and 3-methylglutaric acid in the urine, with various presentations ranging from mild to severe.
- Barth Syndrome: An X-linked recessive disorder primarily affecting males, characterized by cardiomyopathy, skeletal muscle weakness, neutropenia, and growth delays.
Others
- Diabetes Mellitus and Deafness (MIDD): A subtype of mitochondrial disease characterized by maternally inherited diabetes and sensorineural hearing loss.
- Myoneurogenic Gastrointestinal Encephalopathy (MNGIE): A rare disorder characterized by gastrointestinal dysmotility, cachexia, and neurological symptoms.
Diagnosis and Treatment
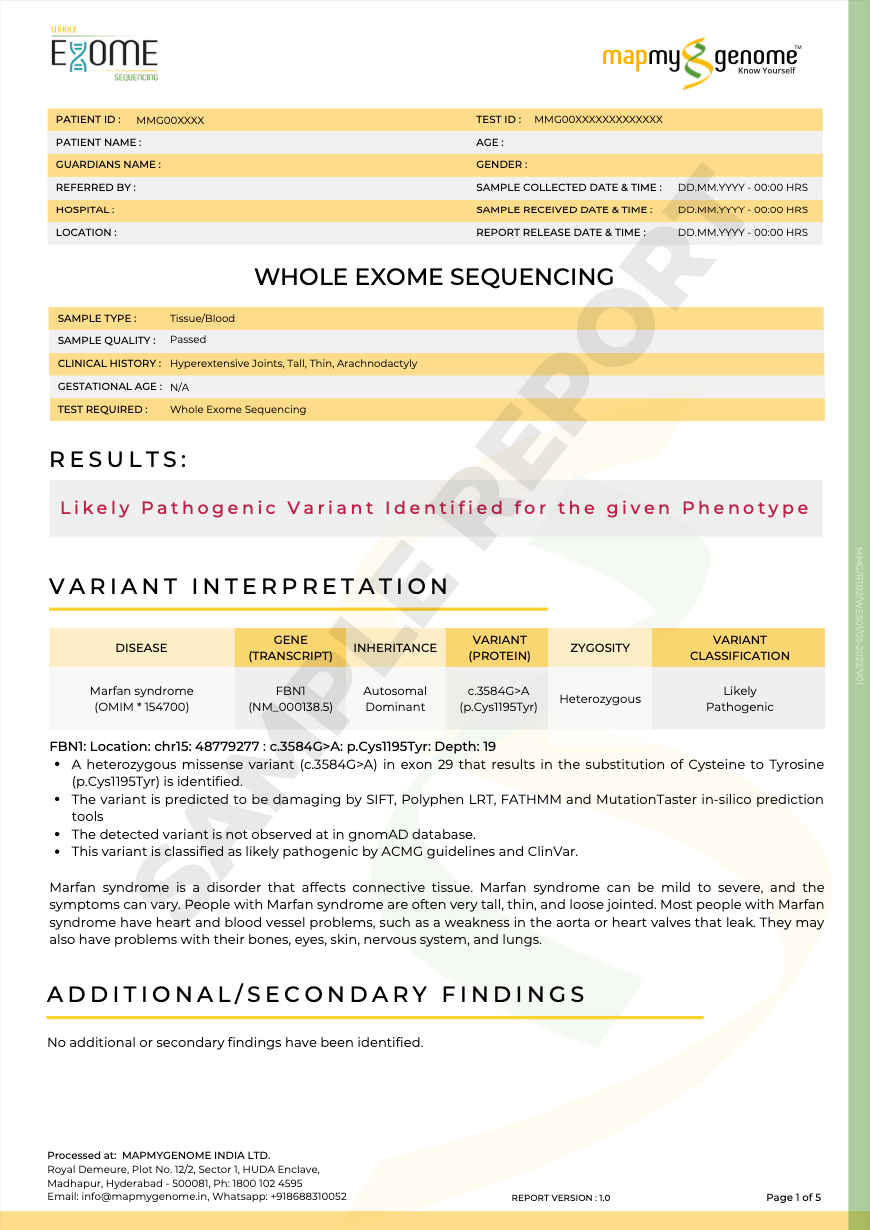
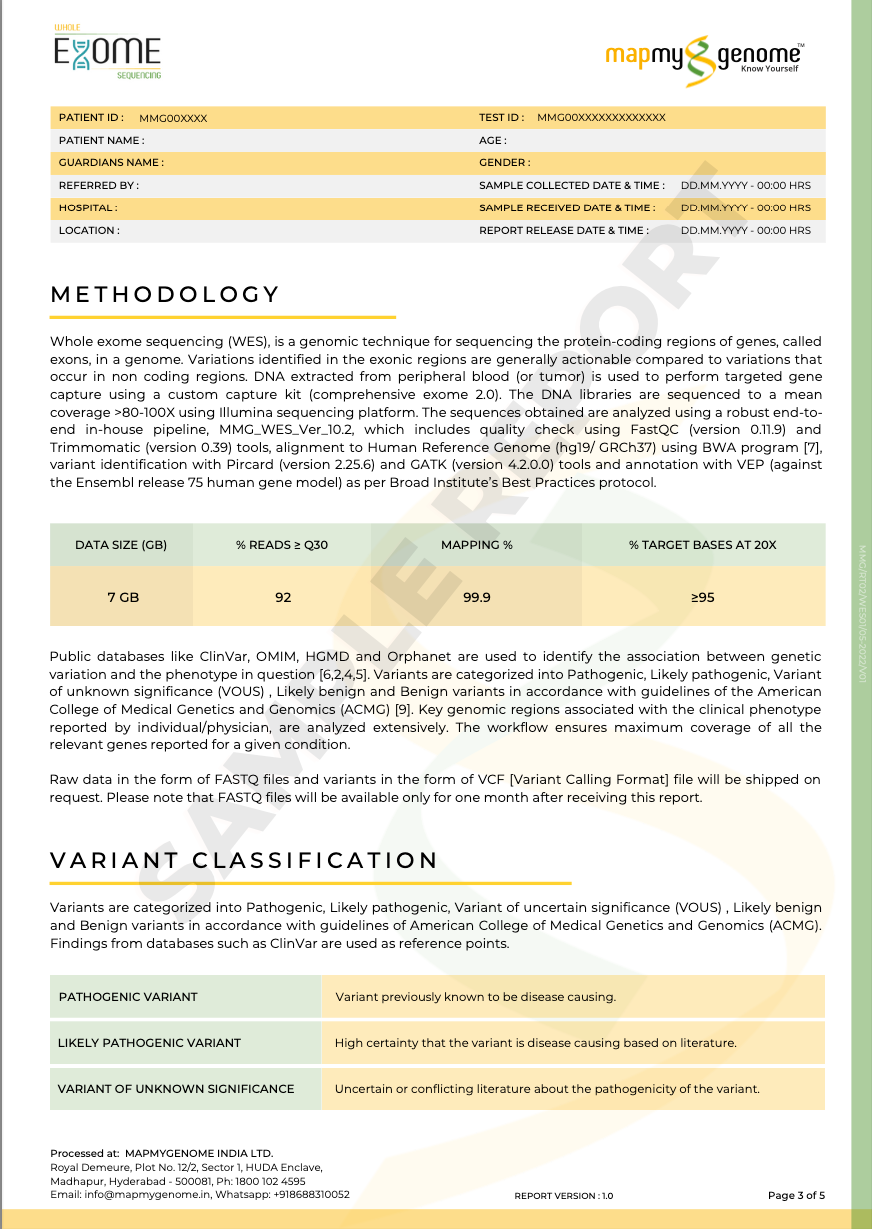
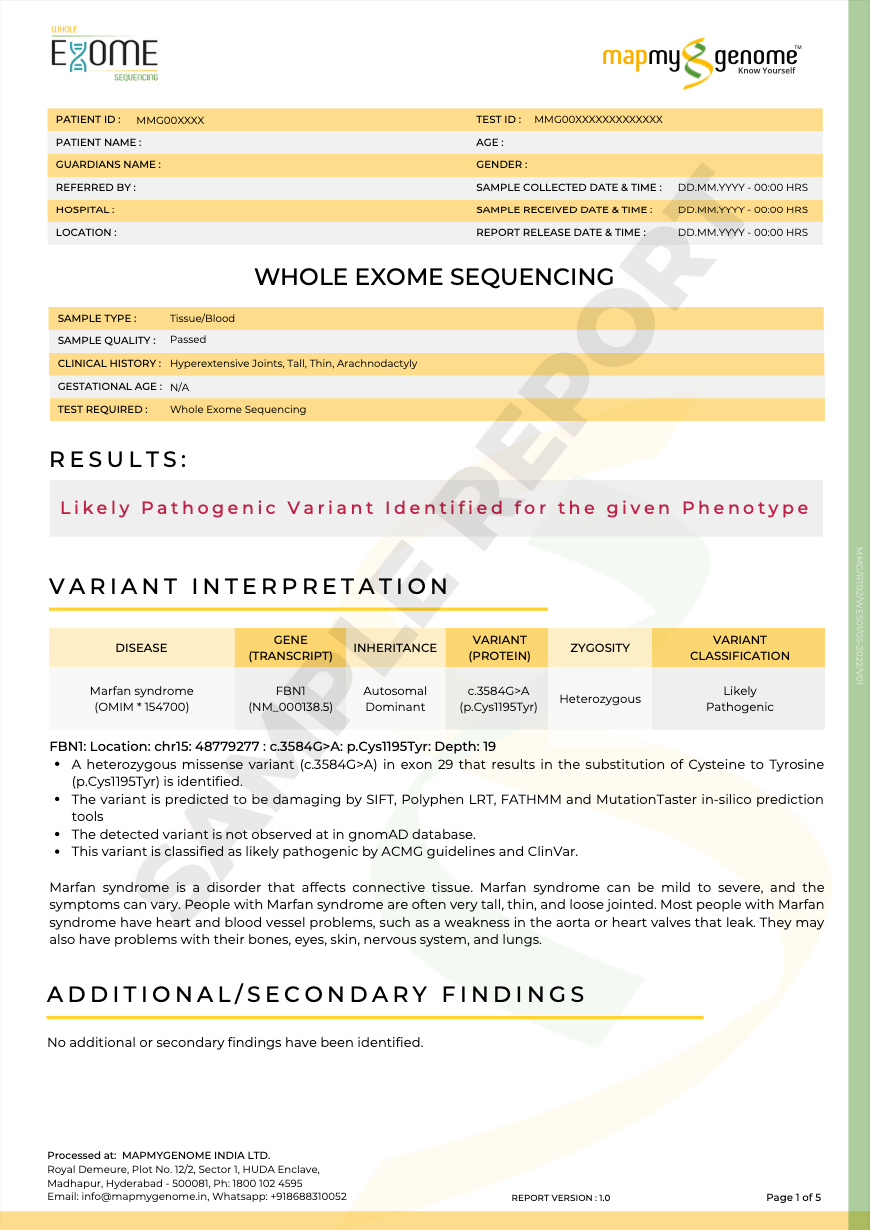
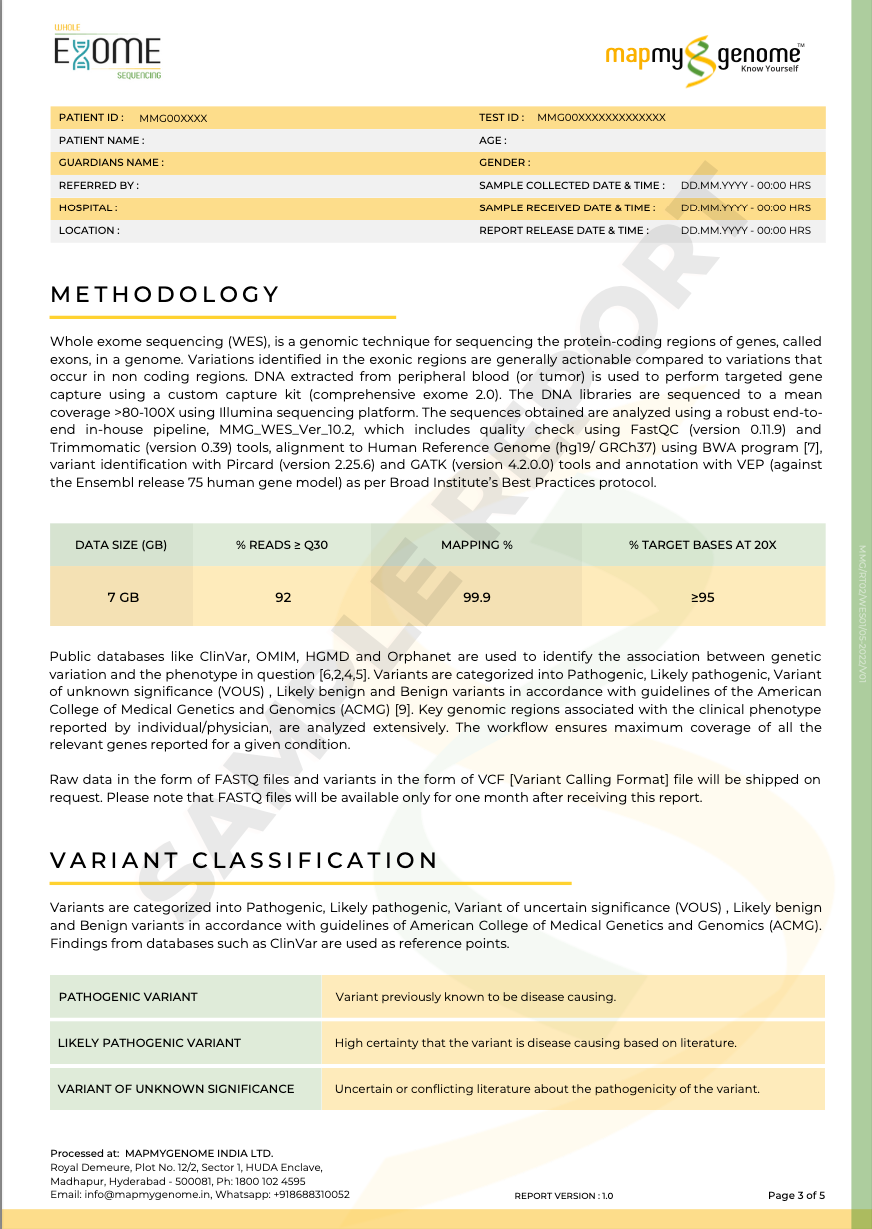
Diagnosing mitochondrial diseases involves a multi-faceted approach:
- Medical history and physical exam: To identify patterns and clues.
- Blood tests: To check for elevated lactate levels, a byproduct of impaired energy production.
- Genetic testing: To identify mutations in mitochondrial or nuclear DNA.
- Muscle biopsy: To examine muscle tissue for signs of mitochondrial dysfunction.
- Specialized imaging: MRI or CT scans to assess organ involvement.
Treatment for mitochondrial diseases focuses on managing symptoms and improving quality of life:
- Medications: To address specific symptoms or enhance mitochondrial function.
- Vitamins and supplements: CoQ10, B vitamins, and other supplements may support mitochondrial health.
- Dietary changes: A balanced diet rich in antioxidants and specific nutrients can be beneficial.
- Physical therapy: To maintain muscle strength and mobility.
- Occupational therapy: To assist with daily living activities.
- Experimental therapies: Gene therapy, mitochondrial replacement therapy, and other novel approaches are being investigated.
Conclusion
Mitochondrial diseases are a complex and diverse group of disorders, each with its unique set of challenges. However, through ongoing research and advancements in medical science, new treatment options and therapies are continually emerging, offering hope for improved management and quality of life for those affected. By understanding the intricacies of these diseases, we can raise awareness, support those affected, and contribute to a future where individuals with mitochondrial diseases can lead fulfilling lives.