हमारा हृदय शरीर में रक्त पंप करने के लिए अथक प्रयास करता है, जिससे हर कोशिका को जीवन देने वाली ऑक्सीजन मिलती है। लेकिन कभी-कभी, रुकावटें रक्त प्रवाह को रोक सकती हैं, जिससे दिल के दौरे जैसी गंभीर स्वास्थ्य जटिलताओं का खतरा बढ़ जाता है। यह ब्लॉग बताएगा कि हृदय की रुकावट क्या है, इसके लक्षण, उपचार और रोकथाम के लिए सुझाव। चाहे आप अपने लिए या किसी प्रियजन के लिए सीखने के लिए यहाँ आए हों, यह मार्गदर्शिका हृदय स्वास्थ्य को समझना सरल और व्यावहारिक बना देगी।
हार्ट ब्लॉकेज क्या है?
हृदय की रुकावट, जिसे कोरोनरी धमनी रुकावट भी कहा जाता है, तब होती है जब धमनियों में वसायुक्त जमाव (प्लाक) जमा हो जाता है, जिससे हृदय की मांसपेशियों में रक्त का प्रवाह मुश्किल हो जाता है। समय के साथ, यह जमाव रक्त प्रवाह को कम या पूरी तरह से अवरुद्ध कर सकता है, जिससे सीने में दर्द, सांस लेने में तकलीफ या यहां तक कि दिल का दौरा जैसी हृदय संबंधी समस्याएं हो सकती हैं।
हृदय की रुकावटें धीरे-धीरे विकसित होती हैं, अक्सर कई सालों तक पता नहीं चलतीं, जब तक कि लक्षण सामने नहीं आ जाते। लेकिन चिंता न करें - समय पर पता लगाने और जीवनशैली में बदलाव करने से काफ़ी फ़र्क पड़ सकता है।
हृदय अवरोध के प्रकार
उनकी गंभीरता और स्थान के आधार पर हृदय रुकावट के विभिन्न प्रकार होते हैं:
- आंशिक रुकावट: धमनी संकरी हो जाती है लेकिन फिर भी कुछ रक्त प्रवाहित हो जाता है। इससे परिश्रम के दौरान सीने में दर्द जैसे हल्के लक्षण हो सकते हैं।
- पूर्ण रुकावट: धमनी पूरी तरह से अवरुद्ध हो जाती है, जिससे आमतौर पर अधिक गंभीर लक्षण उत्पन्न होते हैं और तत्काल चिकित्सा की आवश्यकता होती है।
- इलेक्ट्रिकल हार्ट ब्लॉक: यह एक अलग प्रकार की रुकावट है जिसमें हृदय के विद्युत संकेत विलंबित या बंद हो जाते हैं, जिससे हृदय की धड़कन प्रभावित होती है।
हृदय अवरोध के सामान्य कारण
यद्यपि हृदय अवरोधन जटिल है, फिर भी कुछ सामान्य कारक जोखिम को बढ़ा सकते हैं:
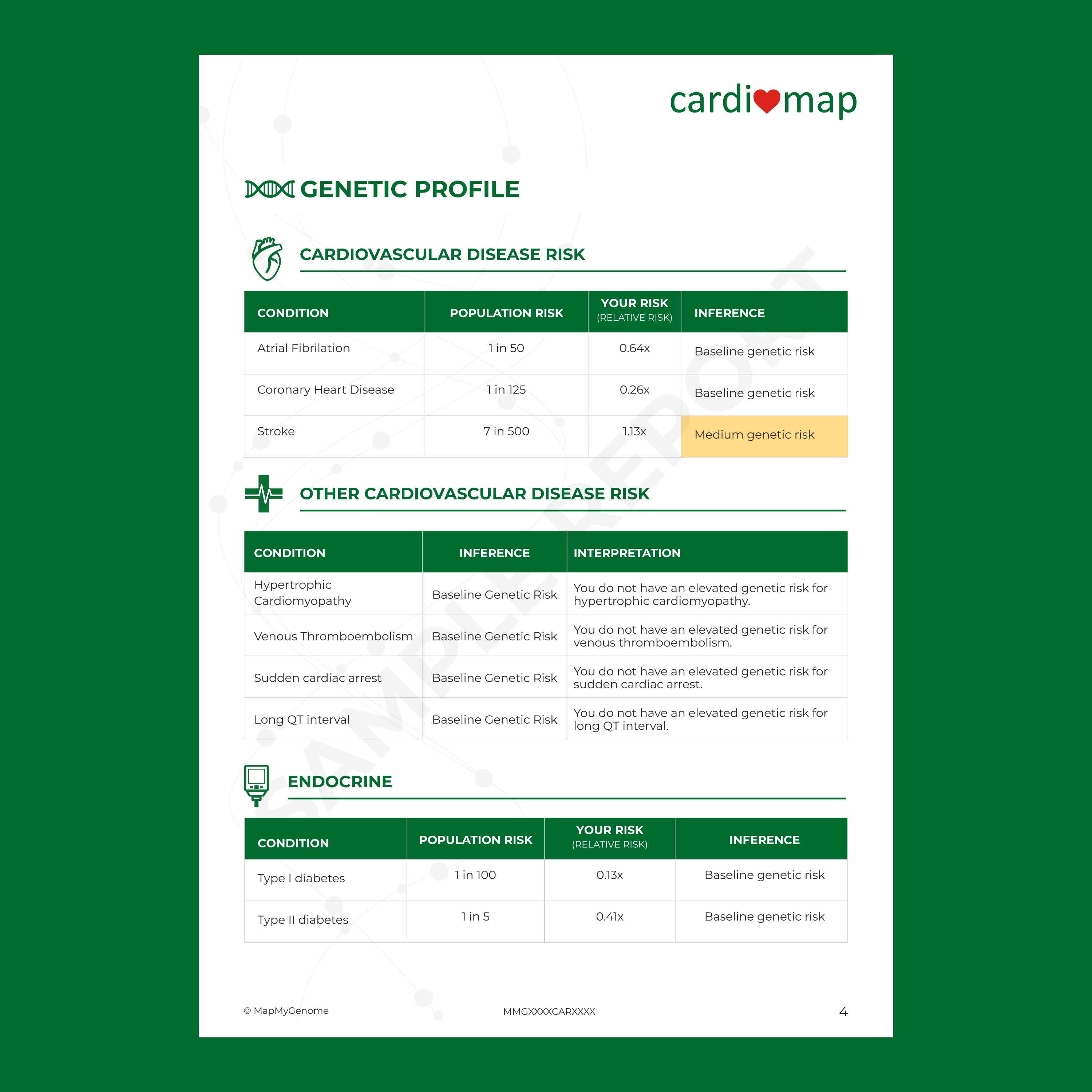
- उच्च कोलेस्ट्रॉल: एलडीएल (खराब कोलेस्ट्रॉल) का उच्च स्तर धमनियों में प्लाक के निर्माण में योगदान देता है।
- उच्च रक्तचाप: उच्च रक्तचाप धमनी की दीवारों को नुकसान पहुंचाता है, जिससे प्लाक का जमा होना आसान हो जाता है।
- धूम्रपान: सिगरेट में मौजूद निकोटीन और अन्य रसायन रक्त वाहिकाओं को नुकसान पहुंचा सकते हैं, जिससे रुकावटें बढ़ सकती हैं।
- मधुमेह: मधुमेह से पीड़ित लोगों की धमनियों में प्लाक बनने की संभावना अधिक होती है।
- अस्वास्थ्यकर आहार: उच्च वसा, उच्च चीनी वाला आहार प्लाक निर्माण में योगदान देता है।
- व्यायाम की कमी: शारीरिक निष्क्रियता रक्तचाप और कोलेस्ट्रॉल बढ़ा सकती है, जिससे प्लाक का निर्माण बढ़ सकता है।
इन कारणों को समझने से आपको जोखिम को कम करने के लिए सूचित जीवनशैली विकल्प चुनने में मदद मिल सकती है।
हृदय अवरोध के लक्षण
हार्ट ब्लॉकेज के हमेशा शुरुआती लक्षण नहीं दिखते, इसलिए इनका पता लगाना मुश्किल हो सकता है। जब लक्षण दिखाई देते हैं, तो उनमें ये शामिल हो सकते हैं:
- सीने में दर्द (एनजाइना): सबसे आम लक्षण, जो अक्सर शारीरिक परिश्रम या तनाव के कारण उत्पन्न होता है।
- सांस लेने में तकलीफ: कम रक्त प्रवाह ऑक्सीजन के स्तर को प्रभावित करता है, जिससे सांस लेने में तकलीफ होती है।
- थकान: अवरुद्ध धमनी के कारण साधारण कार्य भी थका देने वाला हो सकता है।
- पसीना आना: अत्यधिक पसीना आना, विशेष रूप से न्यूनतम गतिविधि के दौरान, एक चेतावनी संकेत हो सकता है।
- मतली या चक्कर आना: इन्हें कभी-कभी नजरअंदाज कर दिया जाता है लेकिन ये हृदय संबंधी समस्या का संकेत हो सकते हैं।
यदि आप या कोई अन्य व्यक्ति इन लक्षणों का अनुभव करता है, विशेष रूप से सीने में दर्द या सांस लेने में तकलीफ, तो तुरंत चिकित्सा सहायता लें।
हृदय अवरोध का निदान
डॉक्टर हृदय की रुकावटों का निदान करने के लिए कई तरीकों का इस्तेमाल करते हैं। कुछ सामान्य परीक्षण इस प्रकार हैं:
- इलेक्ट्रोकार्डियोग्राम (ईसीजी): हृदय में विद्युतीय गतिविधि को मापता है, असामान्य लय का पता लगाता है।
- इकोकार्डियोग्राम: इसमें ध्वनि तरंगों का उपयोग करके हृदय का विस्तृत चित्र बनाया जाता है, तथा रुकावटों को दर्शाया जाता है।
- तनाव परीक्षण: यह परीक्षण शारीरिक गतिविधि के दौरान आपके हृदय की कार्यप्रणाली की जांच करता है, जिससे अंतर्निहित समस्याओं का पता चल सकता है।
- कोरोनरी एंजियोग्राफी: धमनियों में डाई इंजेक्ट करके अवरोधों को दर्शाने वाला एक विशेष एक्स-रे।
- सीटी या एमआरआई: किसी रुकावट के स्थान और सीमा को देखने के लिए हृदय का विस्तृत स्कैन।
परीक्षण करवाने से रुकावटों का शीघ्र पता लगाने में मदद मिल सकती है, जिससे गंभीर जटिलताओं से बचा जा सकता है।
हृदय अवरोधों के लिए उपचार विकल्प
एक बार निदान हो जाने के बाद, उपचार रुकावट की गंभीरता और समग्र स्वास्थ्य पर निर्भर करता है। आम उपचारों में शामिल हैं:
1. दवाएँ
दवाएँ रक्त प्रवाह को बेहतर बना सकती हैं और प्लाक के और अधिक जमा होने के जोखिम को कम कर सकती हैं। इनमें शामिल हैं:
- कोलेस्ट्रॉल कम करने वाली दवाएं: धमनियों में प्लाक को कम करती हैं।
- रक्त पतला करने वाली दवाएं: थक्के बनने से रोकने में मदद करती हैं।
- बीटा-ब्लॉकर्स या एसीई अवरोधक: रक्तचाप कम करते हैं और हृदय की रक्षा करते हैं।
2. एंजियोप्लास्टी और स्टेंटिंग
आंशिक रुकावटों के मामलों में, एंजियोप्लास्टी की सिफारिश की जा सकती है। धमनी को खोलने के लिए एक छोटे गुब्बारे का उपयोग किया जाता है, और इसे खुला रखने के लिए एक स्टेंट (एक छोटी ट्यूब) लगाया जाता है। इससे रक्त प्रवाह बहाल होता है और लक्षण कम होते हैं।
3. कोरोनरी धमनी बाईपास ग्राफ्ट (सीएबीजी)
गंभीर रुकावटों के लिए, सर्जरी की आवश्यकता हो सकती है। CABG शरीर के किसी अन्य भाग से रक्त वाहिका का उपयोग करके रक्त प्रवाह के लिए एक नया मार्ग बनाता है। यह अवरुद्ध क्षेत्र को बायपास करता है, जिससे हृदय में रक्त प्रवाह में सुधार होता है।
4. जीवनशैली में बदलाव
कई लोगों के लिए, जीवनशैली में बदलाव करके आगे की रुकावटों को रोका जा सकता है और समग्र हृदय स्वास्थ्य में सुधार किया जा सकता है। डॉक्टर अक्सर उपचार के हिस्से के रूप में संतुलित आहार, नियमित व्यायाम, धूम्रपान छोड़ने और तनाव प्रबंधन की सलाह देते हैं।
हृदय की रुकावटों को कैसे रोकें
अपने दिल की देखभाल करना मुश्किल नहीं है। रुकावटों को रोकने में मदद करने के लिए यहाँ कुछ कारगर सुझाव दिए गए हैं:
- हृदय-स्वस्थ आहार अपनाएँ: फलों, सब्जियों, साबुत अनाज और लीन प्रोटीन पर ध्यान दें। ट्रांस वसा, शर्करा युक्त खाद्य पदार्थ और अत्यधिक नमक से बचें।
- सक्रिय रहें: सप्ताह के अधिकांश दिनों में कम से कम 30 मिनट व्यायाम करने का लक्ष्य रखें। पैदल चलना, साइकिल चलाना और तैरना सभी बेहतरीन विकल्प हैं।
- शराब का सेवन सीमित करें: अत्यधिक शराब पीने से रक्तचाप बढ़ सकता है, जिससे हृदय संबंधी समस्याएं हो सकती हैं।
- धूम्रपान छोड़ें: धूम्रपान आपकी धमनियों को नुकसान पहुंचाता है और हृदय में रुकावट का खतरा काफी हद तक बढ़ जाता है।
- तनाव को नियंत्रित करें: लगातार तनाव दिल को नुकसान पहुंचा सकता है। योग या ध्यान जैसी विश्राम तकनीकों का अभ्यास करें।
- नियमित जांच करवाएं: नियमित जांच से जोखिम कारकों को शुरू में ही पकड़ने में मदद मिल सकती है, जिससे आप निवारक उपाय कर सकते हैं।
कुछ छोटे-छोटे बदलाव आपके हृदय को स्वस्थ रखने में काफी मददगार साबित हो सकते हैं।
हृदय अवरोध के बारे में अक्सर पूछे जाने वाले प्रश्न
1. हृदय में रुकावट के शुरुआती लक्षण क्या हैं?
आम लक्षणों में सीने में दर्द, सांस लेने में तकलीफ और अत्यधिक पसीना आना शामिल है। हालांकि, कुछ लोगों में हल्के लक्षण या बिल्कुल भी लक्षण नहीं दिख सकते हैं।
2. क्या हृदय की रुकावटों को प्राकृतिक रूप से ठीक किया जा सकता है?
यद्यपि आप गंभीर रुकावटों को पूरी तरह से ठीक नहीं कर सकते, लेकिन आहार और व्यायाम जैसे जीवनशैली में परिवर्तन करके रक्त प्रवाह में सुधार किया जा सकता है और प्लाक के निर्माण को कम किया जा सकता है, जिससे आगे की रुकावटों को रोका जा सकता है।
3. हृदय की रुकावट का पता कैसे लगाया जाता है?
हृदय में रुकावट का पता ईसीजी, इकोकार्डियोग्राम, तनाव परीक्षण, कोरोनरी एंजियोग्राफी और सीटी या एमआरआई स्कैन जैसे परीक्षणों के माध्यम से लगाया जा सकता है।
4. क्या हृदय की रुकावट के लिए सर्जरी ही एकमात्र विकल्प है?
नहीं, हमेशा नहीं। दवाइयाँ, जीवनशैली में बदलाव और एंजियोप्लास्टी जैसी प्रक्रियाएँ हल्के या आंशिक रुकावटों के लिए पर्याप्त हो सकती हैं। सर्जरी आमतौर पर गंभीर मामलों के लिए की जाती है।
5. एंजियोप्लास्टी के बाद स्टेंट कितने समय तक चलता है?
स्टेंट कई सालों तक चल सकता है, लेकिन नई रुकावटों को रोकने के लिए जीवनशैली में बदलाव ज़रूरी है। अपने डॉक्टर से नियमित रूप से मिलते रहना भी ज़रूरी है।
6. क्या हृदय में रुकावट के कारण दिल का दौरा पड़ सकता है?
हां, हृदय में रुकावट के कारण हृदय की मांसपेशियों में रक्त का प्रवाह कम हो सकता है, जिसका समय पर उपचार न होने पर दिल का दौरा पड़ सकता है।
अंतिम विचार: अपने हृदय स्वास्थ्य की जिम्मेदारी लें
हृदय की रुकावटें गंभीर हो सकती हैं, लेकिन जरूरी नहीं कि वे आपके जीवन को परिभाषित करें। जीवनशैली में छोटे-छोटे सार्थक बदलाव करके आप अपने जोखिम को कम कर सकते हैं, और चिकित्सा प्रगति के साथ, उपचार पहले से कहीं बेहतर हैं। याद रखें, अपने हृदय स्वास्थ्य की जिम्मेदारी लेने में कभी देर नहीं होती।
अगर आपको कोई लक्षण या जोखिम कारक नज़र आते हैं, तो अपने डॉक्टर से बात करने में संकोच न करें और नियमित जांच करवाएं। जब बात दिल की हो, तो रोकथाम हमेशा इलाज से बेहतर होती है।