Lately, the heartbreaking news of celebrities and seemingly healthy young individuals collapsing due to sudden cardiac arrest has left many people feeling anxious and confused. How can someone who looks fit and active fall victim to such a devastating event without warning?
Cardiac arrest occurs in 4 to 14 per 100 000 apparently healthy young adults aged 18 to 40 years worldwide each year. In India specifically, studies have shown an estimated survival of less than 10%, out of hospital cardiac arrest remains one of the leading causes of death. Due to the recent trend of increased prevalence of cardiac arrest in young adults and plausible role of COVID vaccine increased risk for cardiac arrests, studies by the Indian Council of Medical Research (ICMR) and National Centre for Disease Control (NCDC) affirm that COVID-19 vaccines in India are safe and effective, with extremely rare instances of serious side effects.
The ICMR and NCDC have been working together to understand the causes behind sudden unexplained deaths, especially in young adults between the ages of 18 and 45 years. To explore this, two complementary studies were undertaken using different research approaches—
-
One based on past data and another involving real-time investigation. The first study, conducted by ICMR’s National Institute of Epidemiology (NIE), was titled “Factors associated with unexplained sudden deaths among adults aged 18-45 years in India – A multicentric matched case–control study.” This study was carried out from May to August 2023 across 47 tertiary care hospitals in 19 states and Union Territories. It looked at individuals who appeared to be healthy but died suddenly between October 2021 and March 2023. The findings have conclusively shown that COVID-19 vaccination does not increase the risk of unexplained sudden death in young adults.
-
The second study, titled “Establishing the cause in sudden unexplained deaths in young,” is currently being conducted by the All India Institute of Medical Sciences (AIIMS), New Delhi with funding and in collaboration with ICMR. This is a prospective study aimed at determining the common causes of sudden deaths in young adults. Early analysis of data from the study indicates that heart attacks, or myocardial infarction (MI), continue to be the leading cause of sudden death in this age group. Importantly, no major changes in the pattern of causes have been observed when compared with previous years.
Lifestyle vs gene or both?
Based on autopsy studies, 55% to 69% of young adults who die after a cardiac arrest have
-
a heart rhythm disorder (most common in athletes)
-
structural heart disease such as coronary artery disease
-
hypertrophic cardiomyopathy (abnormally thickened heart muscle).
Complex, multifactorial conditions can increase the risk for SCA:
Coronary artery abnormalities:
Defects in the coronary arteries’ connection to the heart may result in decreased blood supply to the heart muscle during exercise, causing cardiac arrest. Usually congenital, young people with this condition may not experience symptoms until they are older.
Myocarditis:
Triggered by infection, myocarditis causes inflammation of the heart walls. Most cases occur when a virus affects the heart, but bacterial, fungal, or parasite infections and allergic reactions to medications can also cause Myocarditis.
Coronary atherosclerosis
Rising incidence of coronary atherosclerosis in young people. It is no more a disease of the elderly . Heart attacks and SCA among youngsters are increasing due to (ADD IN A BOX)
-
Sedentary lifestyles
-
Diabetes
-
Alcohol consumption
-
Substance abuse
-
Smoking
-
Obesity
-
Irregular sleep cycles
-
High-stress work environments
-
Hypertension
These factors can heighten the risk of SCA or also lead to other medical conditions and complications.
Electrolyte Imbalances
Electrolytes are vital for body chemistry to function correctly. Potassium, calcium and sodium are the most important electrolytes. Electrolyte abnormalities are commonly associated with cardiovascular emergencies. These abnormalities may cause or contribute to cardiac arrest.
Genetic conditions, caused by single gene changes can increase risk for developing SCA:
Hypertrophic cardiomyopathy:
Often inherited and undiagnosed, hypertrophic cardiomyopathy is the most common cardiovascular cause of SCA in young people. Thickened muscle cells in the heart’s lower chambers can lead to abnormal heart rhythms, particularly during intense exercise.
Primary arrhythmias:
In those with structurally normal hearts, SCA can sometimes be caused by undiagnosed genetic conditions affecting the heart’s electrical impulses. These include inherited conditions like:
-
Long QT syndrome – a heart rhythm condition causing rapid, chaotic heartbeats.
-
Brugada syndrome- is a rare, inherited heart condition that can cause potentially fatal arrhythmias (abnormal heart rhythms). It's characterized by specific electrocardiogram (ECG) patterns and an increased risk of sudden cardiac arrest, particularly in structurally normal hearts.
-
Arrhythmogenic right ventricular dysplasia (ARVD) – is an inherited condition where heart muscle tissue gets replaced with scar tissue.
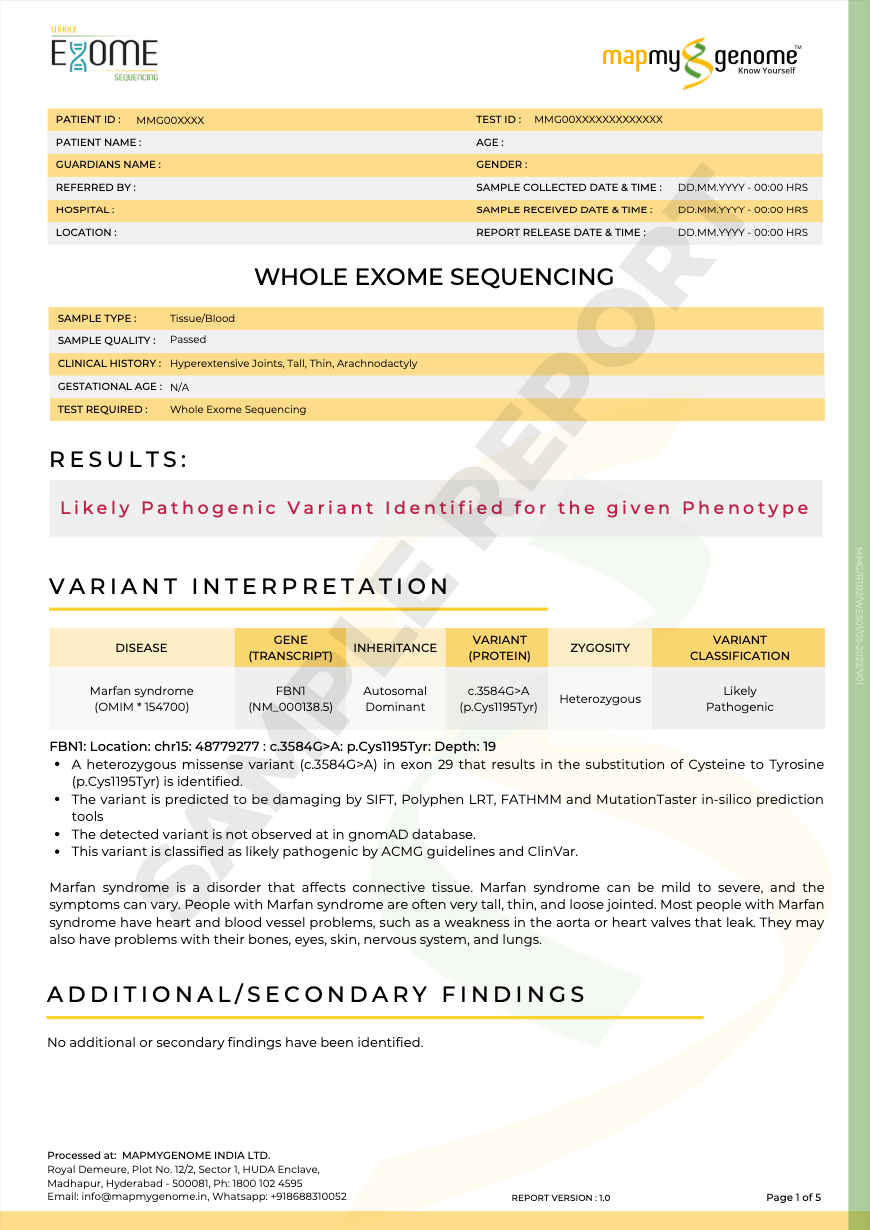
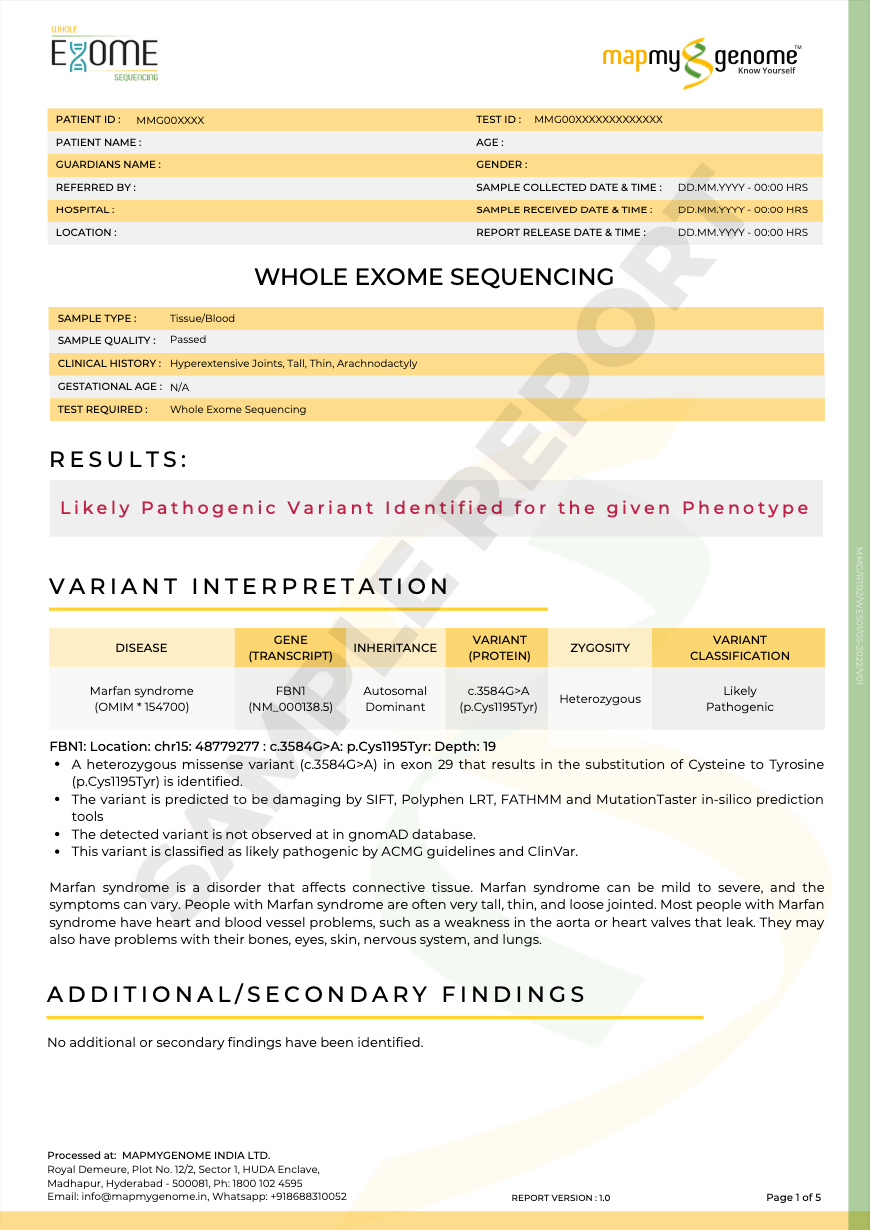
Marfan syndrome
This connective tissue disease can result in tears in the aorta.
Genetic predisposition - SNPs vs genetic mutation
Shifting focus to predisposition
The studies by ICMR and AIIMs have shown that In the majority of the unexplained death cases, genetic mutations have been identified as a possible cause of these deaths.
Monogenic risk variants are rare genetic changes found in less than 1% of the population. These changes usually cause major disruptions in how genes work and can significantly increase the risk of certain diseases. They follow clear inheritance patterns, meaning they are passed down in families in predictable ways (known as Mendelian inheritance).
Some examples include mutations in the LDLR, APOB, and PCSK9 genes, which can cause familial hypercholesterolemia (FH)—a condition marked by very high cholesterol levels and a higher risk of early heart attacks.
In contrast, polygenic risk variants are more common (found in at least 1% of the population) and each contributes a small amount to disease risk.
As stated by the American Heart Association in their guidelines in 2022:
Incorporation of genetics into risk prediction frameworks offers the opportunity to refine risks, potentially earlier in life, toward the creation of earlier and tailored risk reduction strategies.
What actionable steps can I take to know my genetic risks?
Genomepatri is an advanced, at-home DNA-based health and wellness test created by Mapmygenome. The test provides a comprehensive genetic assessment covering over 100 health-related conditions, including detailed risks for cardiovascular diseases (CVDs), metabolic disorders, cancers, and more.
Genomepatri evaluates your genetic predisposition to several heart-related conditions, including but not limited to:
-
Coronary artery disease
-
Myocardial infarction (heart attack)
-
Atrial fibrillation
-
Hypertrophic cardiomyopathy
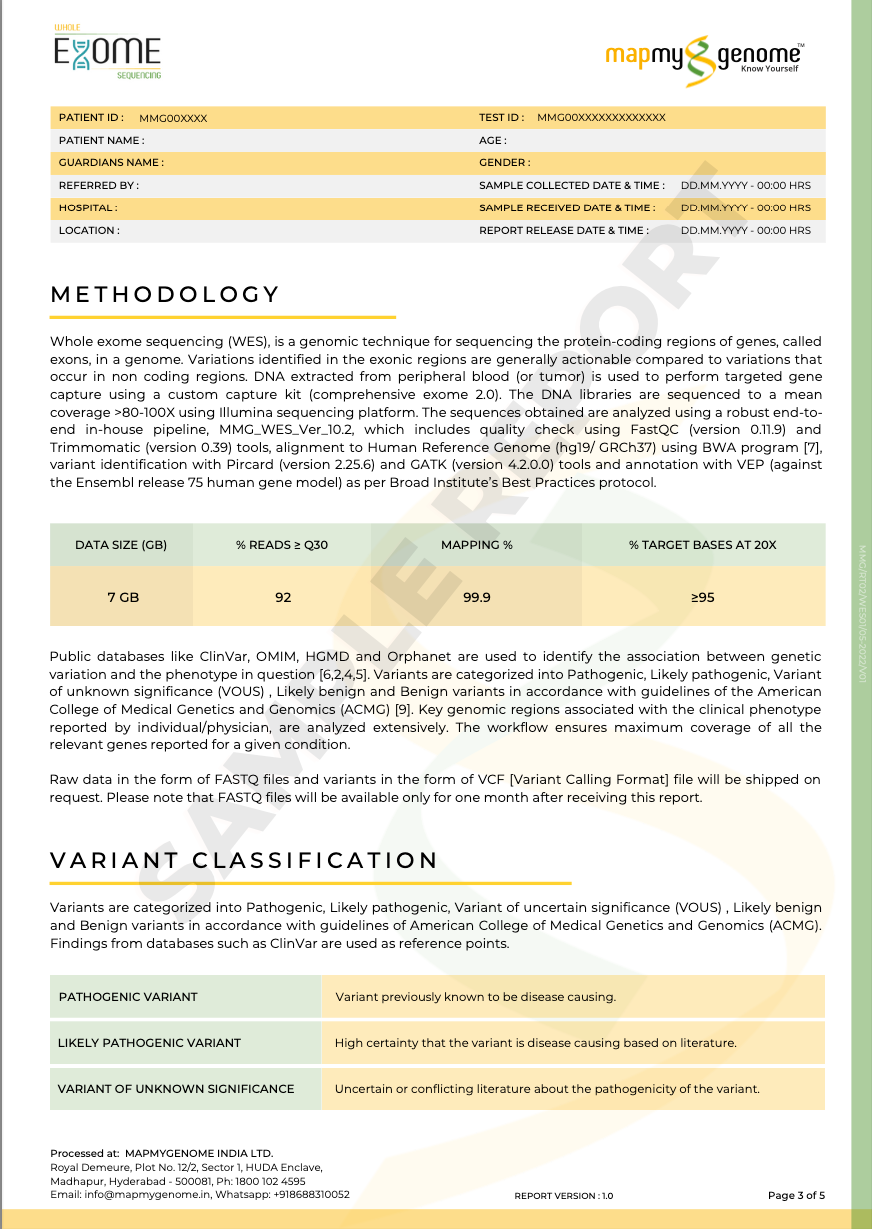
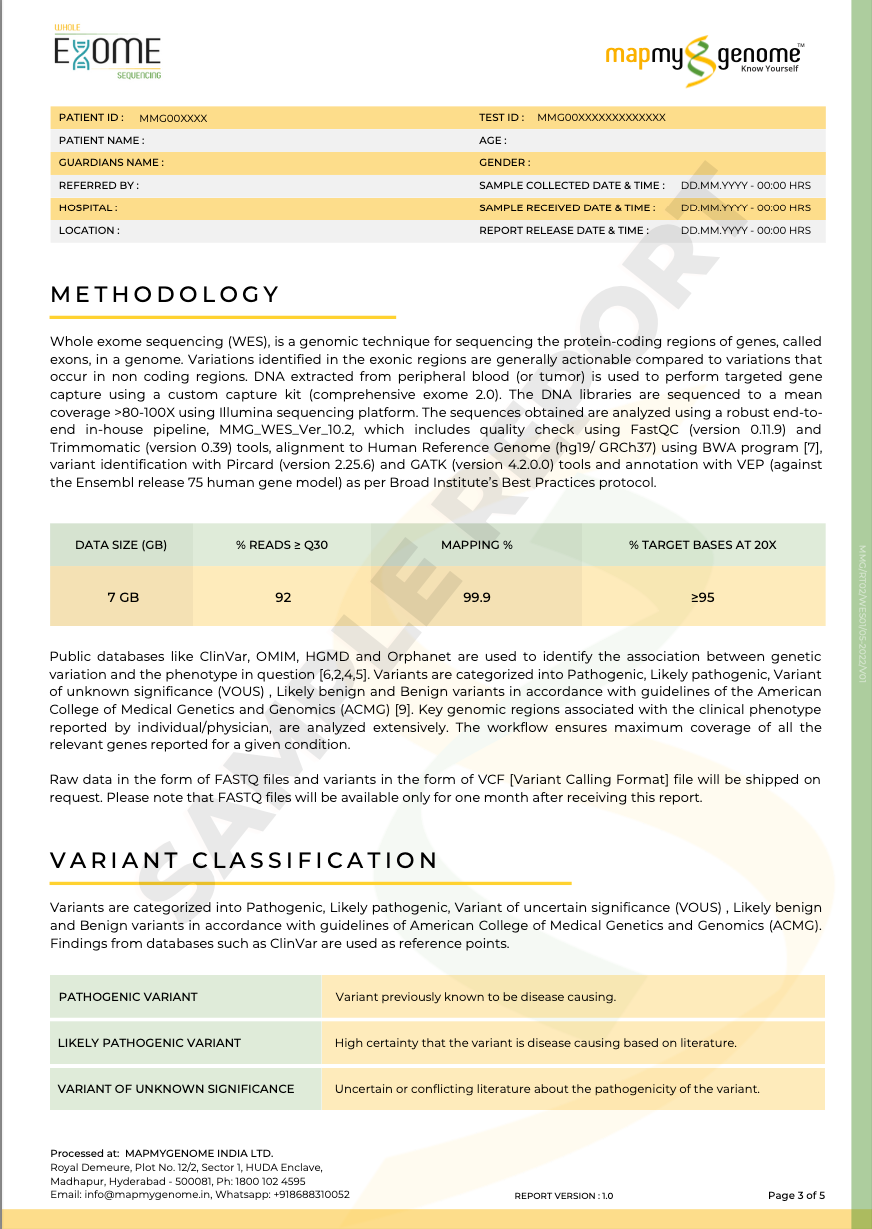
Diagnostic genetic testing such as a cardiomyopathy panel, arrhythmia panel or clinical/whole exome sequencing is recommended for patients suspected of hereditary cardiac disease.
Pharmacogenomic polygenic risk scores (PRSs) are used in four main ways:
-
To predict how well a drug will work (efficacy),
-
To predict the risk of side effects (toxicity),
Medicamap helps individuals understand how their genetic makeup influences their response to various medications, enabling doctors to prescribe safer and more effective drugs.
Red flags for diagnostic genetic test include
Family history of sudden cardiac death, unexplained fainting, or known genetic heart disease- multiple family members with sudden cardiac arrest in the absence of other comorbidities
Unexplained syncope (fainting) or seizures, especially during exertion or emotion
Congenital or structural heart defects in the patient or family- Includes conditions such as hypertrophic or dilated cardiomyopathy, Marfan syndrome, or arrhythmogenic right ventricular cardiomyopathy
Signs in babies and young children: Cyanosis (blue lips/skin), rapid breathing, failure to thrive, swelling, or repeated fainting episodes
Is knowing the end or a new beginning?
Learning of the genetic risk factors can help you tailor your diet and lifestyle and reduce risk factors. It also allows you to personalize your medical screening to specifically address risk factors. Lifestyle that can help reduce the risk of developing sudden cardiac arrest include:
-
Eating a healthy diet with plenty of fruits, vegetables, whole grains, lean proteins, and limited saturated fats, sugar, and salt.
-
Regular physical activity and exercise to maintain heart health and a healthy weight.
-
Quitting smoking and avoiding tobacco products, as smoking is a major risk factor for heart problems.
-
Managing stress through relaxation techniques, counseling, or lifestyle changes, since stress can contribute to heart disease
-
Following a healthy circadian rhythm—by maintaining regular sleep and wake times, getting enough restorative sleep, and aligning eating and activity patterns with daylight hours—helps reduce risk factors (like high blood pressure, obesity, diabetes, and chronic stress) that contribute to the development of heart rhythm disturbances